IUI Procedure Step by Step Guide
In the realm of addressing infertility, the dual dimensions of “perplexity” and “burstiness” play a pivotal role.
The former intricately delves into the convoluted nature of the text, while the latter appraises the diversity within sentences. Human authors typically exhibit heightened burstiness, seamlessly weaving short and protracted sentences.
Conversely, the sentences produced by artificial intelligence tend to embody a uniform length. To craft content that boasts an optimal level of perplexity and burstiness, it’s imperative to bear these considerations in mind.
Furthermore, when venturing into the creation of written content, artificial intelligence often employs lexicons that diverge from the nuanced choices made by human wordsmiths. The integration of unconventional terminology serves as a catalyst, elevating the uniqueness of the composition.
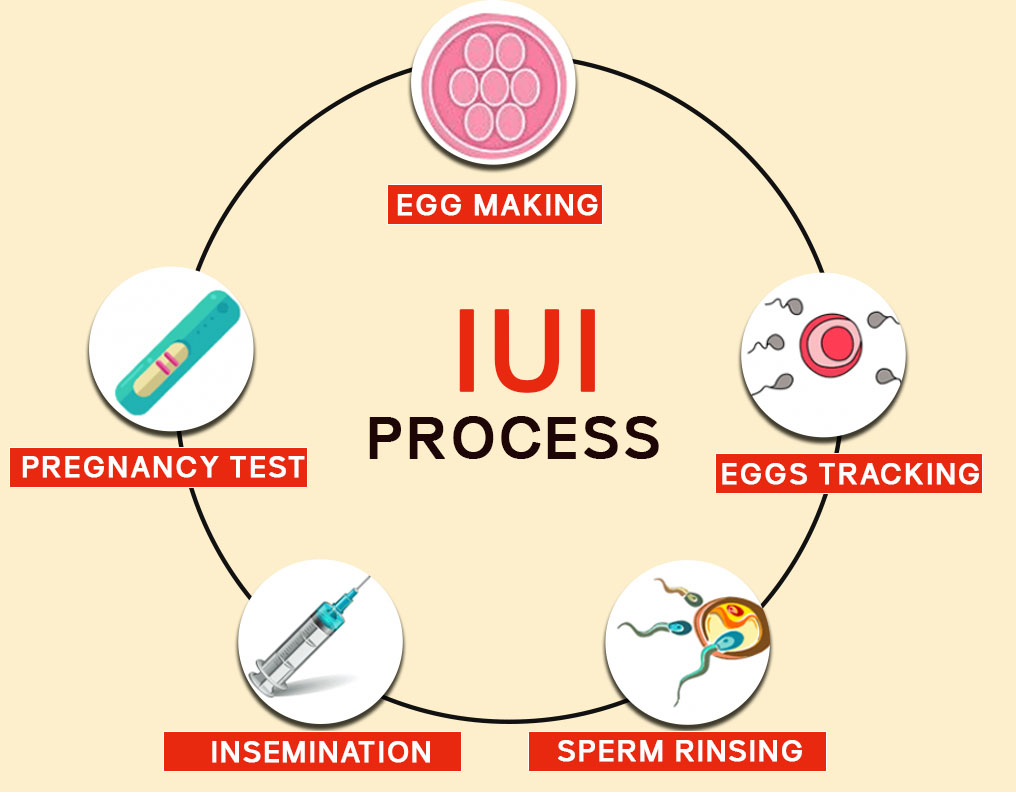
In the domain of fertility treatment, Intrauterine Insemination (IUI) emerges as a pivotal procedure. This technique amplifies the prospects of conception by strategically depositing meticulously prepared sperm directly into the uterus, the crucible for fetal development. An alternate nomenclature for this process is artificial insemination.
With IUI, sperm insertion aligns with the release of eggs from the ovary. The desired outcome is the union of sperm and egg within the fallopian tube, the vital conduit linking the uterus and ovaries. The fruition of this fusion heralds the onset of pregnancy.
The orchestration of Intrauterine Insemination can harmonize with the rhythms of an individual’s menstrual cycle. This cycle, marked by the periodic release of an egg from either of the two ovaries, can also be synchronized with fertility medications to stimulate egg production.
The selection of the method hinges on the specific etiology of infertility.
Products & Services
Why it’s pursued
The fecundity of couples or individuals is contingent upon multifarious factors. Intrauterine Insemination finds prevalence in scenarios involving:
1.Donor Sperm: An option for singles, those with partners lacking viable sperm, or those facing low sperm quality. Certified lab-sourced donor sperm, thawed pre-procedure, is the conduit for conception.
2.Unexplained Infertility: Frequently, IUI serves as the inaugural intervention for inexplicable infertility, often augmented by ovulation-stimulating medications.
3.Endometriosis-Linked Infertility: Tissue resembling uterine lining growing outside the uterus can impede fertility. Initial recourse involves medications and IUI to secure a robust egg.
4. Mild Male Factor Infertility (Subfertility): Impaired semen, scrutinized through a semen analysis, may hinder conception. IUI, by segregating high-quality sperm, surmounts this impediment.
5.Cervical Factor Infertility: Anomalies in the cervix, such as thickened mucus or scarring, can obstruct sperm’s trajectory. IUI circumvents these hurdles by depositing sperm directly into the uterus.
6.Ovulatory Factor Infertility: Individuals grappling with ovulatory irregularities may opt for IUI to address deficiencies in egg release.
7.Semen Allergy: An uncommon allergic reaction to seminal proteins, circumvented by IUI to facilitate pregnancy without triggering adverse symptoms.
Potential Risks
While often deemed a straightforward and low-risk procedure, Intrauterine Insemination carries potential pitfalls:
1.Infection: A minimal risk of post-IUI infection exists.
2.Spotting: The catheter insertion during IUI may induce minor vaginal bleeding, termed spotting, with negligible impact on pregnancy likelihood.
3.Multiple Pregnancy: While IUI per se doesn’t escalate the odds of multiple pregnancies, when coupled with fertility medications, the risk increases, necessitating vigilance for associated complications.
Preparation Protocols
IUI necessitates meticulous preparatory steps:
1.Ovulation Monitoring: Crucial for timing, monitoring ovulation signs using home kits or transvaginal ultrasound is imperative. Hormonal interventions like human chorionic gonadotropin (HCG) may be administered.
2.Strategic Timing: The procedure is typically scheduled a day or two post-ovulation indications.
3.Semen Sample Processing: Partner-provided or donor sperm undergoes washing, isolating highly active, healthy sperm for concentrated effectiveness.
Procedure Overview
The IUI procedure unfolds in a clinical setting, involving minimal time and no need for analgesics. The steps include:
1.Preparation: Patient assumes a supine position with legs in stirrups. A speculum opens the vaginal walls.
2.Catheter Insertion: A catheter, affixed to a vial housing healthy sperm, traverses the vagina, cervix, and reaches the uterus.
3.Sperm Deposition: The sperm sample transits through the catheter into the uterus.
4.Conclusion: Catheter removal precedes speculum retrieval. Post-procedure, a brief recumbent period ensues, with resumption of daily activities thereafter. Light spotting may occur temporarily.
Post-Procedure Anticipation
Allow a fortnight before attempting an at-home pregnancy test to circumvent:
False-Negatives: Inadequate pregnancy hormone levels might yield misleading negative results.
False-Positives: Lingering fertility medication traces could spur inaccurate positive outcomes.
Subsequent to the home test, a follow-up, involving potential blood tests, unfolds approximately two weeks later. For those unsuccessful, revisiting IUI for 3 to 6 cycles remains a viable option before exploring alternative fertility avenues.
Conclusion
Intrauterine Insemination (IUI) emerges as a promising solution in the intricate landscape of fertility treatments. Its meticulous orchestration, synchronizing with menstrual cycles and addressing diverse infertility factors, positions it as a valuable option.
While the procedure is generally considered safe, potential risks necessitate awareness. The strategic use of IUI, coupled with advanced monitoring and processing techniques, offers hope to those navigating the challenging path of conception.
