Reproductive Technologies: Unanticipated Ramifications, Perils, and Financial Investment
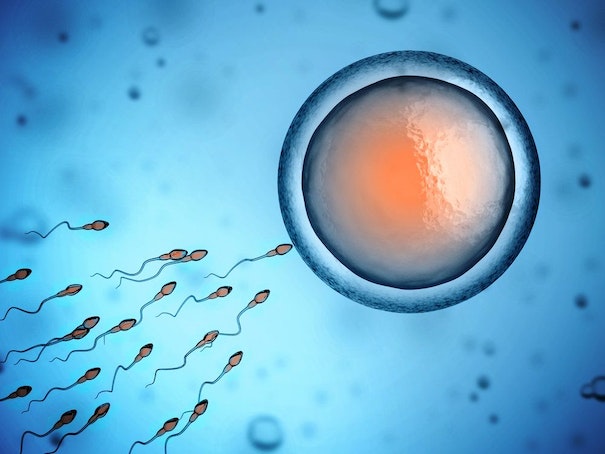
Reproductive technologies, such as intracervical insemination (ICI) and intrauterine insemination (IUI), heighten the chances of conception. Delve into the intricacies of these fertility procedures, exploring their methodologies, financial implications, and success metrics.
Tracing its roots back to the 1700s, reproductive technologies encompass procedures for achieving pregnancy without engaging in sexual intercourse. This can involve donor sperm or specifically chosen genetic material. For instance, couples facing fertility challenges may resort to sperm banks, a common practice. However, the adoption of artificial insemination is not exclusive to couples; it is a viable option for single individuals and those in same-sex relationships.
Here’s an exhaustive exploration of two prevalent reproductive technologies: intrauterine insemination (IUI) and intracervical insemination (ICI), encompassing procedural intricacies and overall expenditures.
Unraveling Reproductive Technologies
Reproductive technologies represent fertility interventions introducing sperm directly to the cervix or uterus. Achieved through intrauterine insemination (IUI) or intracervical insemination (ICI), the primary objective is to facilitate pregnancy.
Decoding the Mechanism—and Optimal Scheduling
Artificial insemination follows a schedule aligned with the individual’s menstrual cycle. Coordination with ovulation, occurring approximately 14 days before menstruation, maximizes the likelihood of success. Consequently, artificial insemination is a once-per-cycle endeavor.
Ovulation verification involves blood and urine tests, as well as at-home ovulation kits. There are two methods of artificial insemination; delve deeper to grasp the specifics of IUI and ICI.
Intrauterine Insemination (IUI)
Preferred for male-factor infertility, IUI is versatile, addressing unexplained infertility and endometriosis-induced challenges. Thick cervical mucus hindering sperm-egg interaction is also a scenario where IUI proves beneficial.
Commencing the IUI process involves elevating fertility through medications. The subsequent preparation of a semen sample, either from the intended father or a donor, involves separating sperm from seminal fluid to mitigate uterine contractions. The catheter-based insertion of sperm into the uterus mirrors a Pap smear. The direct uterine deposition reduces the sperm’s travel distance, elevating the chances of conception. Dr. Tanmoy Mukherjee estimates IUI success rates per cycle as follows:
– 8 to 10% for male-factor infertility
– 5% for tubal infertility
– 18 to 20% for unexplained infertility
Intracervical Insemination (ICI)
A simpler method mimicking natural intercourse, ICI involves injecting unwashed, liquefied semen into the vagina using a specialized syringe. The individual aspiring for pregnancy should recline for about 30 minutes post-procedure. Success rates range from 5% to 30% per cycle, potentially improving with a sponge cap over the cervix or sperm washing. ICI is also known as Intravaginal Insemination (IVI).
Unveiling Side Effects
Individual reactions to artificial insemination vary. Some may experience cramping and light bleeding, while others remain unaffected.
Navigating Risks
Although the risks associated with IUI and ICI are minimal, complications may arise. Common risks include pelvic infections, ovarian hyperstimulation syndrome (OHSS), and an increased likelihood of multiple pregnancies when fertility medications are involved.
Financial Considerations
Intrauterine insemination costs range from $300 to $1,000 per cycle without insurance. Donor sperm incurs additional charges, ranging from $700 to $1,000 per vial. Health insurance may cover ancillary expenses like blood work, ultrasounds, and medications.
On the contrary, intracervical insemination costs approximately $200 to $350 per cycle. Unwashed sperm contributes to the lower cost, while washed sperm and donor options increase expenses. Given the modest success rates of IUI and ICI, multiple cycles are often necessary. In cases of persistent failure, in vitro fertilization (IVF) becomes an alternative. This process involves combining sperm and eggs in a petri dish before implanting the resulting embryo into the uterus, costing around $15,000. Despite the higher expense, IVF boasts a greater success rate (approximately 53.9% for those under 35 using fresh eggs).
This narrative, while addressing both male and female fertility aspects, acknowledges the diverse identities of individuals undergoing fertility treatments.
