Did you know that around one in ten women experience PCOS (polycystic ovary syndrome)? This condition is among the leading causes of infertility for women. PCOS comes with a variety of hormonal symptoms, including irregular periods, acne, and unwanted body hair. Unfortunately, many women go undiagnosed for years, and the condition can often be misdiagnosed due to its complex nature. To shed light on PCOS, the popular site Refinery29 reached out to Dr. Emily Carter, a board-certified reproductive endocrinologist, to share her insights on getting pregnant with PCOS.
Dr. Carter explains, “PCOS is polygenetic,” meaning it’s not caused by a single gene defect like cystic fibrosis or sickle cell disease. Instead, it involves multiple genes that, for reasons still unclear, don’t function well together.
Understanding the Link Between PCOS and Fertility
While PCOS is well known for its impact on fertility, Dr. Carter notes that the focus on reproductive issues is largely due to the fact that gynecologists were among the first to identify the disorder. Because PCOS affects various body systems, she believes the name “PCOS” can be misleading. For example, the disorder can affect insulin levels, leading to weight gain—a symptom not directly related to fertility. Some women may only experience metabolic issues while others might only have reproductive symptoms, suggesting that a more descriptive name could clarify the condition.
When it comes to fertility, PCOS can significantly hinder the development of ovarian follicles, which are crucial for ovulation. Dr. Carter points out that women with PCOS often have multiple small follicles that don’t mature properly, preventing the release of a viable egg for fertilization. She likens these undeveloped follicles to cars stuck at a traffic light, unable to move forward.
Tips for Getting Pregnant with PCOS
Despite being a common cause of infertility, the encouraging news is that many women with PCOS achieve pregnancy with the right treatment. A personalized approach often begins with less invasive options like oral medications such as Clomid or Letrozole, which help stimulate follicle development. If these methods aren’t effective, injectable gonadotropins may be used, along with timed intercourse for better chances of conception.
For those who still find it challenging to conceive, intrauterine insemination (IUI) is another viable option. Research shows that women with PCOS, especially those under 35, often have success with IUI.
Weight management can be a struggle for women with PCOS, as they face an increased risk of infertility and miscarriage. Exercise has been shown to improve fertility outcomes, and it’s not just about losing weight; it’s about incorporating a consistent exercise routine.
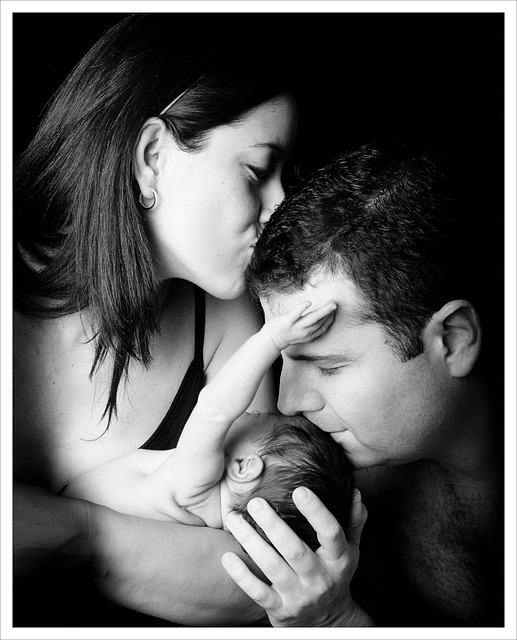
The emotional aspect of dealing with PCOS shouldn’t be overlooked either. Sharing experiences and discussing challenges can alleviate stress. Remember, you are not alone in this journey.
If you’re interested in learning more about the path to parenthood, check out our heartfelt post about finding joy through home insemination. Additionally, for comprehensive information about pregnancy, visit the CDC’s pregnancy resource page. And if you’re considering home insemination, you might want to explore some kits available at this trusted provider.
Summary
PCOS affects a significant number of women and can complicate the journey to parenthood. With the right treatments and support, many women can successfully conceive. It’s essential to understand the complexities of PCOS, including its effects on fertility and overall health. If you’re looking for more guidance on your path to parenthood, there are resources available to help you navigate this journey.